Clinical Definition
Diabetes Mellitus (DM) is a group of chronic metabolic disorders characterized by persistent hyperglycemia (elevated blood glucose) resulting from defects in insulin secretion, insulin action, or both. The condition is broadly classified into Type 1 Diabetes (T1DM), an autoimmune destruction of pancreatic beta-cells leading to absolute insulin deficiency, and Type 2 Diabetes (T2DM), characterized by peripheral insulin resistance and progressive beta-cell dysfunction. Uncontrolled DM leads to microvascular and macrovascular complications.
Clinical Coding & Classification
| System / Category | Code(s) | Description |
|---|---|---|
| ICD-10-CM | E10.9 | Type 1 diabetes mellitus without complications |
| ICD-10-CM | E11.9 | Type 2 diabetes mellitus without complications |
| CPT (Lab) | 83036 | Hemoglobin; glycosylated (A1C) |
| CPT (Device) | 95250 | Ambulatory continuous glucose monitoring (CGM) of interstitial tissue fluid |
| Affected System | Endocrine; Metabolic | Pancreatic Islets of Langerhans |
Epidemiology & Statistics
According to the International Diabetes Federation (IDF) Diabetes Atlas, approximately 1 in 10 adults worldwide live with diabetes. T2DM accounts for over 90% of all cases, strongly correlated with the global prevalence of obesity and sedentary lifestyles. T1DM usually presents in childhood or adolescence but can occur at any age. The economic burden is driven largely by the management of chronic complications (renal, retinal, cardiovascular).
Pathophysiology (Mechanism)
The underlying mechanisms differ by type but converge on hyperglycemia:
1. Type 1 (Autoimmune): T-cell mediated destruction of insulin-producing beta-cells in the pancreatic islets. Autoantibodies (e.g., anti-GAD, anti-IA2) are typically present.
2. Type 2 (Resistance + Dysfunction):
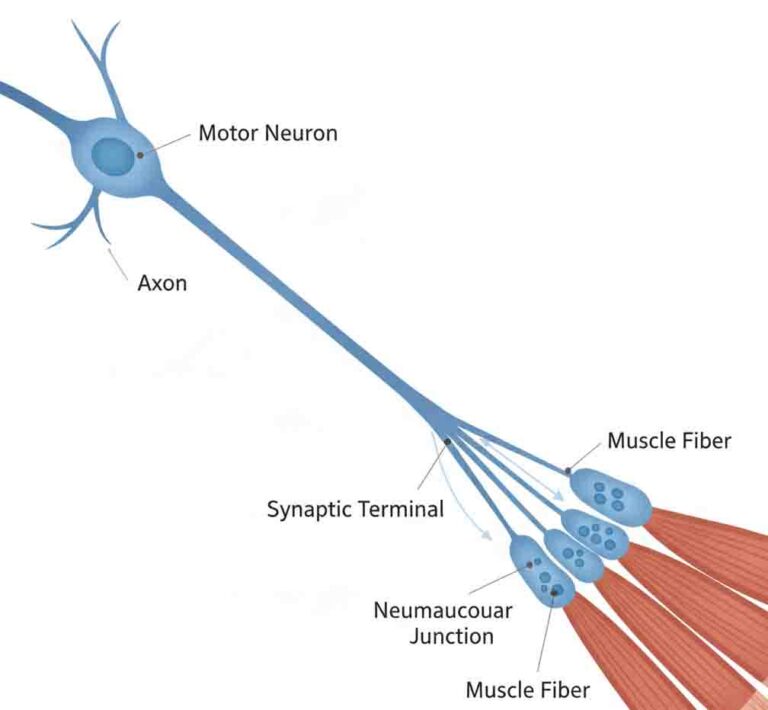
– Insulin Resistance: Decreased glucose uptake in skeletal muscle and adipose tissue, and increased hepatic glucose production.
– Beta-cell Dysfunction: Progressive failure of beta-cells to compensate for the resistance, exacerbated by glucotoxicity and lipotoxicity.
Standard Management Protocols
Therapeutic goals focus on glycemic control (HbA1c targets) and cardiovascular risk reduction.
- Pharmacological Classes:
- Biguanides: (e.g., Metformin) The first-line therapy for T2DM; reduces hepatic glucose production.
- SGLT2 Inhibitors: (e.g., Empagliflozin) Inhibit renal glucose reabsorption; noted for cardiorenal protective benefits.
- GLP-1 Receptor Agonists: (e.g., Semaglutide, Liraglutide) Incretin mimetics that enhance insulin secretion, delay gastric emptying, and promote weight loss.
- Insulin Therapy: (Basal/Bolus) Essential for survival in T1DM and used in advanced T2DM.
- Technology & Procedures:
- Continuous Glucose Monitoring (CGM): Real-time monitoring of interstitial glucose levels.
- Bariatric Surgery: Considered for T2DM patients with BMI >35 kg/m².
Healthcare Resource Utilization
Diabetes is a primary driver of healthcare costs due to multisystem complications:
- Microvascular: Screening for Diabetic Retinopathy (ophthalmology), Diabetic Nephropathy (nephrology/dialysis), and Neuropathy (podiatry/amputation prevention).
- Macrovascular: Aggressive management of hypertension and dyslipidemia to prevent Myocardial Infarction and Stroke.