Clinical Definition
Legionnaires’ disease is a severe form of atypical pneumonia caused by the gram-negative, aerobic bacterium Legionella pneumophila. It is acquired primarily through the inhalation of aerosolized water droplets containing the bacteria. Unlike community-acquired pneumonia caused by Streptococcus pneumoniae, Legionnaires’ disease presents with distinctive extrapulmonary manifestations (e.g., diarrhea, hyponatremia) and requires specific antimicrobial coverage due to the pathogen’s intracellular replication capability.
Clinical Coding & Classification
| System / Category | Code(s) | Description |
|---|---|---|
| ICD-10-CM | A48.1 | Legionnaires’ disease |
| ICD-10-CM | A48.2 | Nonpneumonic Legionnaires’ disease (Pontiac fever) |
| CPT (Lab) | 87449 | Infectious agent antigen detection by EIA (Legionella pneumophila) |
| CPT (Lab) | 87540 – 87542 | Infectious agent detection by nucleic acid (DNA), Legionella pneumophila |
| Affected System | Respiratory; Environmental | Pulmonary Alveoli |
Epidemiology & Statistics
Legionella is prevalent in natural and man-made freshwater environments. Outbreaks are frequently associated with complex water systems in hotels, hospitals, and cruise ships (e.g., cooling towers, hot tubs). Risk factors include advanced age (>50), smoking history, and immunocompromised status. Mortality rates for nosocomial (hospital-acquired) infections can reach up to 25% without timely treatment.
Pathophysiology (Mechanism)
The pathogenesis is driven by the bacterium’s ability to survive and replicate intracellularly:
1. Inhalation & Phagocytosis: Aerosolized bacteria reach the alveoli and are phagocytosed by alveolar macrophages.
2. Phagosome Evasion: L. pneumophila prevents the fusion of the phagosome with the lysosome (inhibiting bactericidal activity) and recruits mitochondria and endoplasmic reticulum to create a specialized replicative vacuole.
3. Cytolysis: Bacterial proliferation leads to macrophage rupture, releasing cytokines that trigger a severe inflammatory response and consolidating pneumonia.
Standard Management Protocols
Treatment requires antibiotics with high intracellular penetration. Beta-lactams (e.g., Penicillin, Cephalosporins) are ineffective.
- Pharmacological Classes:
- Fluoroquinolones: (e.g., Levofloxacin, Moxifloxacin) High bioavailability and excellent lung tissue penetration. Often the first-line therapy.
- Macrolides: (e.g., Azithromycin) Effective alternative, particularly for community-acquired cases.
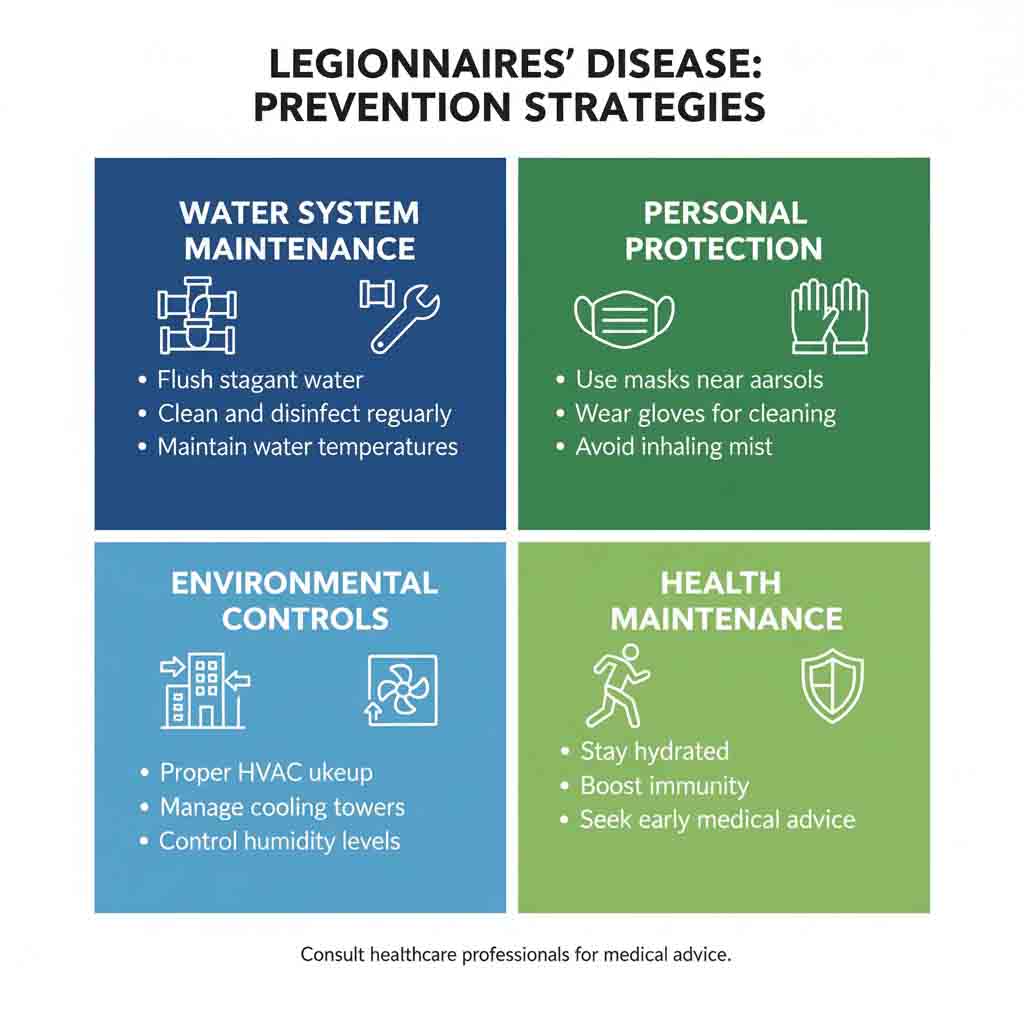
- Environmental Control (B2B/Industrial):
- Water System Maintenance: Routine cleaning of cooling towers and decorative fountains.
- Superheating/Hyperchlorination: Shock treatment of water systems to eradicate biofilm colonization.
Healthcare Resource Utilization
Legionnaires’ disease involves significant clinical and environmental resource utilization:
- Diagnostic Intensity: Reliance on Urinary Antigen Testing (UAT) and PCR for rapid diagnosis.
- Critical Care: Severe cases often require ICU admission for respiratory support (mechanical ventilation).
- Public Health Investigation: Confirmed cases often trigger environmental testing of building water systems to locate the source.