Clinical Definition
Fatty Liver Disease, increasingly referred to as Steatotic Liver Disease (SLD), is defined histologically by the accumulation of excess macrovesicular fat (triglycerides) in >5% of hepatocytes. It is clinically categorized into Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD/NAFLD), driven by insulin resistance and metabolic syndrome, and Alcohol-Associated Liver Disease (ALD). The condition exists on a spectrum ranging from simple steatosis (fat accumulation without inflammation) to Metabolic Dysfunction-Associated Steatohepatitis (MASH/NASH), characterized by hepatocyte ballooning, inflammation, and fibrosis.
Clinical Coding & Classification
| System / Category | Code(s) | Description |
|---|---|---|
| ICD-10-CM | K76.0 | Fatty (change of) liver, not elsewhere classified (NAFLD/MASLD) |
| ICD-10-CM | K70.0 | Alcoholic fatty liver |
| ICD-10-CM | K75.81 | Nonalcoholic Steatohepatitis (NASH) |
| CPT (Diagnostic) | 91200 | Liver elastography (FibroScan) measuring stiffness |
| CPT (Lab) | 80076 | Hepatic function panel |
Epidemiology & Statistics
MASLD is the most common chronic liver disease globally, affecting approximately 25-30% of the adult population. The prevalence correlates strongly with the global rise in obesity and Type 2 Diabetes Mellitus. MASH (the progressive form) is rapidly becoming the leading indication for liver transplantation in Western countries, surpassing viral hepatitis.
Pathophysiology (Mechanism)
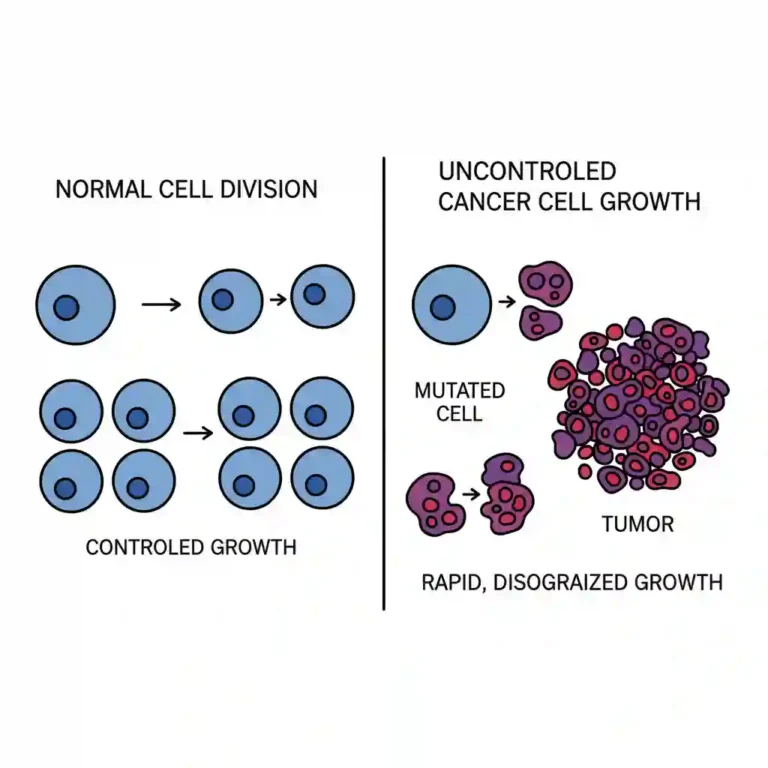
The pathogenesis is described by the “Multiple-Hit Hypothesis”:
1. Insulin Resistance (The First Hit): Peripheral insulin resistance leads to increased lipolysis in adipose tissue, causing a massive influx of Free Fatty Acids (FFAs) to the liver. This overwhelms the liver’s oxidation capacity, leading to triglyceride accumulation (Steatosis).
2. Lipotoxicity & Oxidative Stress (Subsequent Hits): The accumulation of toxic lipid intermediates triggers mitochondrial dysfunction and Reactive Oxygen Species (ROS) production. This induces hepatocyte apoptosis, recruitment of inflammatory cytokines (TNF-alpha, IL-6), and activation of hepatic stellate cells, driving fibrosis.
Standard Management Protocols
Management is multidisciplinary, targeting metabolic risk factors and liver health.
- Pharmacological Classes (Emerging Therapies):
- GLP-1 Receptor Agonists: (e.g., Semaglutide, Liraglutide) Originally for diabetes/obesity, these agents show efficacy in resolving steatohepatitis by promoting weight loss and improving insulin sensitivity.
- Insulin Sensitizers: (e.g., Pioglitazone) Used in select non-diabetic patients with biopsy-proven MASH.
- Antioxidants: (e.g., Vitamin E) Considered for non-diabetic patients to reduce oxidative stress.
- Surgical/Procedural Interventions:
- Bariatric Surgery: (e.g., Sleeve Gastrectomy) Highly effective in resolving steatosis and fibrosis in morbidly obese patients.
Healthcare Resource Utilization
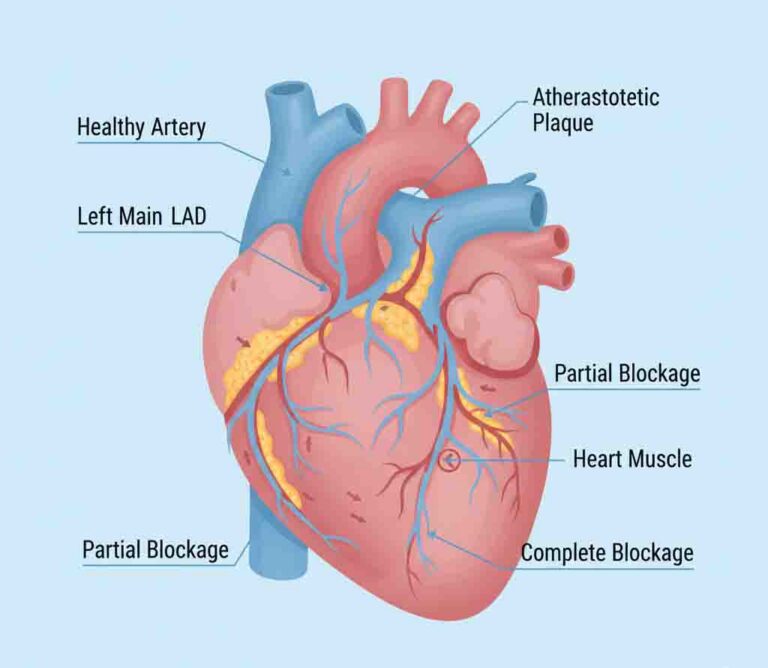
The economic impact of SLD is substantial, primarily driven by:
- Non-Invasive Monitoring: Shift from biopsy to non-invasive biomarkers (FIB-4 Index) and Elastography for fibrosis staging.
- Cardiovascular Comorbidity: The primary cause of mortality in MASLD patients is cardiovascular disease, necessitating extensive cardiac risk management.