Quick Facts: The Language of Your Bill
| Code Type | What It Tells You |
|---|---|
| CPT Code | The Procedure: Tells you what service was provided (e.g., Surgery, X-ray, Office visit). |
| ICD-10 Code | The Diagnosis: Tells you why the service was provided (e.g., High blood pressure, Fracture). |
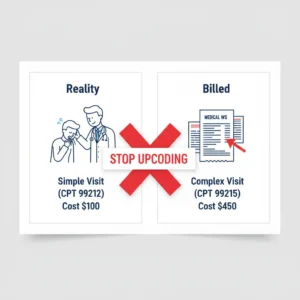
| Upcoding | The illegal practice of using a code for a more expensive service than actually performed. |
| Unbundling | Billing each part of a procedure separately instead of using one all-inclusive code. |
Audit Your Bill: Translating the “Secret” Language
Hospital bills are intentionally difficult to read. By using 5-digit CPT (Current Procedural Terminology) codes instead of plain English, hospitals can obscure what they are actually charging for. If you don’t cross-reference these codes, you could be paying for “complex” care when you only received a “basic” consultation. Auditing these codes is your legal right as a patient and the most direct way to stop medical overcharging.
The “Level 5” Trap: A Common Upcoding Scenario
The most frequent form of upcoding happens in the Emergency Room or during office visits using Evaluation and Management (E/M) codes.
Clinical Scenario: A patient goes to the ER for a minor cut that requires a simple bandage. The visit lasts 15 minutes. No diagnostic tests are ordered.
The Bill: The hospital submits CPT 99285 (ER Visit – High Severity/Complex Decision Making).
The Reality: A 15-minute minor visit should be CPT 99282. The price difference between these two codes can be over $1,500. This is Upcoding.
How to Identify Upcoding and Errors
Follow this 3-step audit protocol to verify your medical charges:
1. Match the Diagnosis (ICD-10) to the Procedure (CPT)
Look at your Explanation of Benefits (EOB). (See also: How to Read an EOB). Does the ICD-10 diagnosis justify the CPT procedure? For example, if your diagnosis is a simple headache (R51.9), but you are being billed for a complex neurological surgery code, you have found a major error.
2. Search for “Unbundled” Charges
In medical billing, “bundles” exist for common procedures. If you had a surgery, the surgical CPT code usually includes the incision, the procedure, and the closing. If the hospital bills you separately for “sutures” or “anesthesia prep” (Unbundling), they are double-charging you.
3. Use an Online CPT Lookup Tool
Once you have your Itemized Bill, enter the CPT codes into a search engine or use the AMA’s CPT lookup tool. Compare the official description of the code with the care you actually received. If the code says “60 minutes of face-to-face time” but the doctor was only with you for 5 minutes, you have leverage for negotiation.
What to Do When You Find an Error
Do not call the “Billing Department” and simply say the bill is high. Use the technical terms you’ve learned. Tell them:
- “I believe there is an E/M coding error on my statement.”
- “I was billed for CPT 99285, but based on the clinical notes, this visit only meets the criteria for 99282.”
- “I request a formal coding review of this account.”
If the insurance company denied your claim because the coding was mismatched, you can use our AI Appeal Letter Generator to help draft a technical rebuttal.
Frequently Asked Questions
Is upcoding illegal?
Yes. Upcoding is considered a form of healthcare fraud. While many hospitals claim it is a “clerical error,” consistent upcoding can lead to massive federal fines for the institution. Patients should never feel intimidated to challenge it.
How can I prove the doctor didn’t spend as much time as the code says?
Request your Medical Records for that visit. The “Clinical Notes” or “Progress Notes” will usually have a time-stamp or a summary of the complexity of the visit. If the notes don’t support a high-level code, the bill must be adjusted.