Clinical Definition
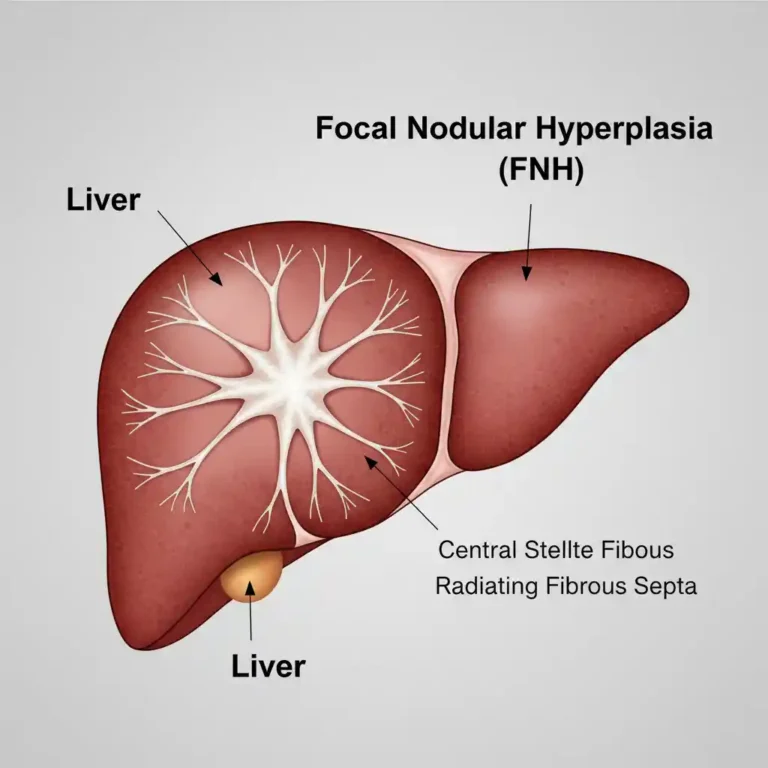
Liver Cirrhosis is the terminal histological stage of various chronic liver diseases, characterized by diffuse hepatic fibrosis and the conversion of normal liver architecture into structurally abnormal nodules (regenerative nodules). This architectural distortion leads to increased intrahepatic resistance, resulting in portal hypertension and synthetic dysfunction. Clinically, the disease trajectory transitions from a “Compensated” state (asymptomatic) to a “Decompensated” state (manifesting as ascites, variceal bleeding, or encephalopathy).
Clinical Coding & Classification
| System / Category | Code(s) | Description |
|---|---|---|
| ICD-10-CM | K74.60 | Unspecified cirrhosis of liver |
| ICD-10-CM | K70.30 | Alcoholic cirrhosis of liver without ascites |
| CPT (Diagnostic) | 91200 | Liver elastography (FibroScan) measuring stiffness |
| CPT (Surgical) | 37182 | Insertion of Transjugular Intrahepatic Portosystemic Shunt (TIPS) |
| Prognostic Score | MELD / Child-Pugh | Scoring systems for transplant prioritization and mortality risk |
Epidemiology & Statistics
Cirrhosis is a leading cause of morbidity and mortality worldwide, accounting for over 1.3 million deaths annually. The primary etiologies vary by region: Chronic Hepatitis B and C are predominant in Asia and Africa, whereas Alcoholic Liver Disease (ALD) and Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD/NAFLD) are leading causes in Western nations. The prevalence of NASH-related cirrhosis is projected to increase exponentially in parallel with the global obesity epidemic.
Pathophysiology (Mechanism)
The central pathogenic mechanism is the activation of Hepatic Stellate Cells (HSCs).
1. Fibrogenesis: Following chronic injury (viral, toxic, or metabolic), quiescent HSCs transdifferentiate into myofibroblasts. These cells secrete excessive extracellular matrix, particularly Collagen Type I and III.
2. Capillarization: The fenestrations of the liver sinusoids are lost (capillarization), impairing the exchange of solutes between plasma and hepatocytes.
3. Portal Hypertension: Structural distortion and vasoconstriction (reduced nitric oxide availability) increase resistance to portal blood flow, driving the formation of portosystemic collaterals (varices) and fluid retention (ascites).
Standard Management Protocols
Management is directed at treating the underlying etiology and preventing complications of portal hypertension.
- Pharmacological Classes:
- Non-Selective Beta-Blockers (NSBBs): (e.g., Propranolol, Carvedilol) Used for primary and secondary prophylaxis of variceal bleeding by reducing portal pressure.
- Diuretics: (e.g., Spironolactone, Furosemide) Standard therapy for managing ascites via aldosterone antagonism.
- Disaccharides/Antibiotics: (e.g., Lactulose, Rifaximin) Used to manage Hepatic Encephalopathy by reducing ammonia absorption.
- Surgical/Procedural Interventions:
- Endoscopic Variceal Ligation (EVL): For acute bleeding or prophylaxis.
- TIPS (Transjugular Intrahepatic Portosystemic Shunt): A radiographic procedure to decompress the portal system in refractory ascites or bleeding.
- Liver Transplantation: The only curative treatment for end-stage decompensated cirrhosis.
Healthcare Resource Utilization
Cirrhosis imposes a massive economic burden driven by repeated hospitalizations and high-cost interventions:
- Readmissions: High rates of 30-day readmission due to Hepatic Encephalopathy and volume overload.
- Transplant Costs: Orthotopic liver transplantation involves significant surgical, immunosuppressive, and long-term surveillance costs.