Clinical Definition
Myocardial Infarction (MI) is defined as acute myocardial cell death (necrosis) due to prolonged ischemia. The “Universal Definition of Myocardial Infarction” classifies the condition based on etiology, distinguishing between Type 1 MI (spontaneous plaque rupture/erosion with thrombosis) and Type 2 MI (ischemic imbalance between oxygen supply and demand). Clinically, it is categorized by electrocardiographic findings into ST-Elevation Myocardial Infarction (STEMI) and Non-ST-Elevation Myocardial Infarction (NSTEMI).
Clinical Coding & Classification
| System / Category | Code(s) | Description |
|---|---|---|
| ICD-10-CM | I21.0 – I21.3 | ST elevation (STEMI) myocardial infarction of specific sites |
| ICD-10-CM | I21.4 | Non-ST elevation (NSTEMI) myocardial infarction |
| CPT (Surgical) | 92928 | Percutaneous Coronary Intervention (PCI) with drug-eluting stent placement |
| CPT (Lab) | 84484 | Troponin, quantitative |
| Affected System | Cardiovascular | Coronary Arteries; Myocardium |
Epidemiology & Statistics
Ischemic heart disease remains the leading cause of mortality globally. In the United States, an MI occurs approximately every 40 seconds. While the incidence of STEMI has declined due to improved preventative management (statins, smoking cessation), the proportion of NSTEMI cases has increased. Mortality rates are significantly higher in patients with comorbidities such as Diabetes Mellitus and Chronic Kidney Disease.
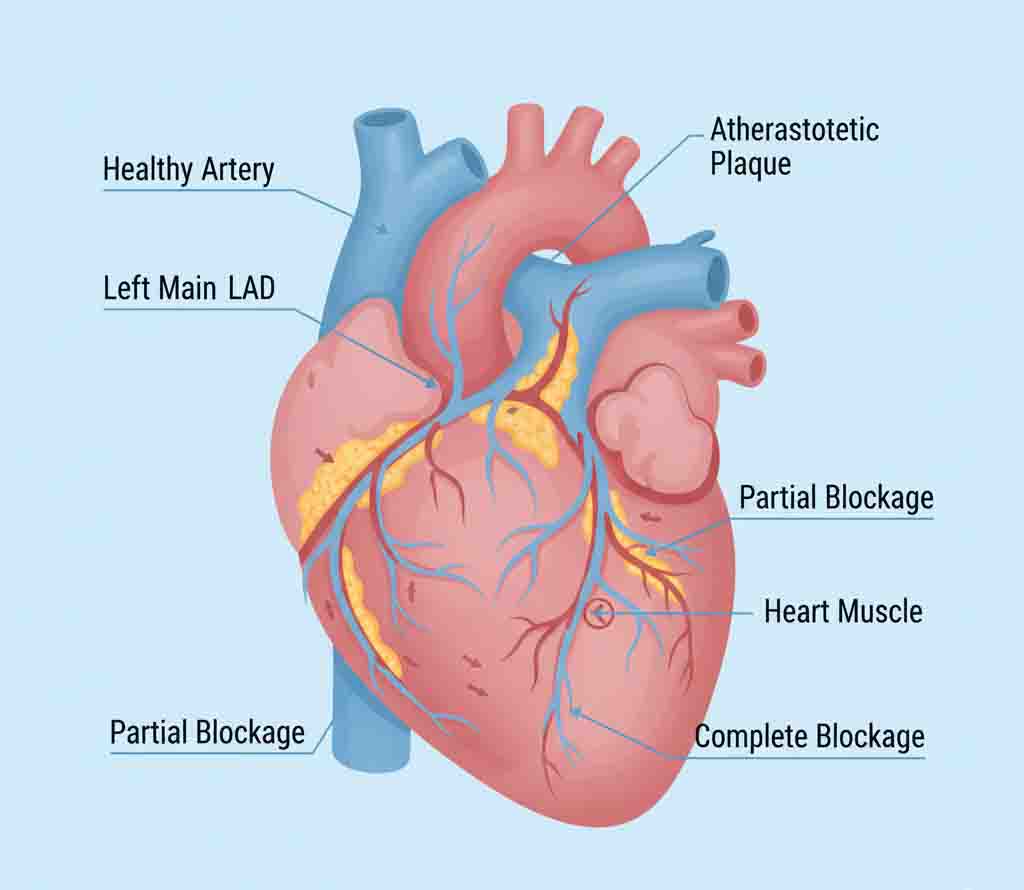
Pathophysiology (Mechanism)
The pathogenesis typically follows the sequence of atherosclerosis progression:
1. Plaque Rupture: An unstable atherosclerotic plaque (thin fibrous cap, lipid-rich core) ruptures, exposing thrombogenic subendothelial matrix.
2. Thrombosis: Platelet activation and aggregation occur rapidly, followed by the activation of the coagulation cascade, forming a thrombus.
3. Occlusion:
– STEMI: Complete, persistent occlusion of a coronary artery leading to transmural necrosis.
– NSTEMI: Partial or intermittent occlusion, or occlusion with collateral circulation, resulting in subendocardial necrosis.
Standard Management Protocols
Immediate management relies on reperfusion strategies and stabilization.
- Reperfusion Therapy:
- Primary PCI: The gold standard for STEMI. Guidelines recommend a “Door-to-Balloon” time of <90 minutes.
- Fibrinolysis: (e.g., Tenecteplase) Indicated only if PCI cannot be performed within 120 minutes of first medical contact.
- Pharmacological Classes:
- Dual Antiplatelet Therapy (DAPT): Aspirin + P2Y12 Inhibitor (e.g., Ticagrelor, Prasugrel, Clopidogrel).
- Anticoagulants: (e.g., Unfractionated Heparin, Bivalirudin) Used during the acute phase.
- Secondary Prevention: High-intensity Statins, Beta-blockers, and ACE Inhibitors/ARBs to prevent remodeling.
Healthcare Resource Utilization
MI management is resource-intensive, focusing on quality metrics:
- Catheterization Lab: High fixed costs associated with 24/7 availability for emergency PCI.
- Cardiac Rehabilitation: A structured outpatient program proven to reduce readmission rates and mortality.